
The CareSource mission is to make a lasting difference in the lives of our members. At the same time, we recognize the importance of our responsibility to state and regulatory stakeholders to manage their funds prudently and responsibly. With recent increased scrutiny into the profit margins of third-party Pharmacy Benefit Managers (PBMs), CareSource created RxInnovations.
Now we can provide not only better pharmacy service for our members, but also better fiscal accountability and efficiency for our stakeholders.
“We believe the current PBM model has significant room for improvement,” said Erhardt Preitauer, President & CEO, CareSource. “CareSource saw an opportunity to reinvent the model with a focus on transparency, driving real value for stakeholders, building stronger partnerships with local pharmacies and controlling costs.”
“This is the culmination of an 18-month effort to address the major areas of opportunity in the current PBM model,” said Don Amorosi, Senior Vice President, Pharmacy, CareSource. “We are creating something that better serves members on their terms through the integration of all data—medical, behavioral, social and pharmacy. This will allow us to provide holistic care coordination, while also meeting the needs of our other key stakeholders—the states in which we do business and our community provider partners.”
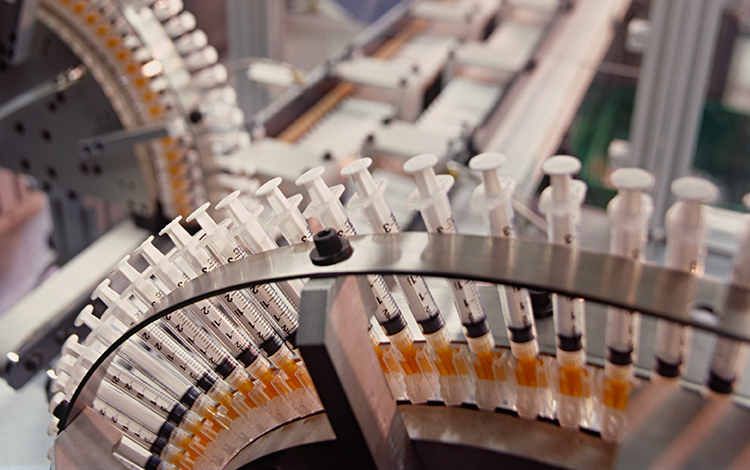
CareSource launched our new pharmacy management program on January 1, 2020. Through CareSource RxInnovations, we can leverage comprehensive data and claims management technology to improve stakeholder alignment and power pharmacy innovation for better health outcomes.

CareSource RxInnovations drives pharmacy savings for states by providing full price transparency validated by an independent third-party. At the same time, it offers complete visibility about how pharmacy dollars are being spent for Medicaid beneficiaries.
Custom pharmacy networks are being designed to provide members the same access and more services, while protecting independent pharmacies from volatility created by the traditional PBM model.
Value-based programs will now drive increased quality of care for the consumer, leveraging incentives to local pharmacists for educating patients and preventing adverse drug events.
Through it all, an integrated, industry-leading data platform will identify real-time opportunities to improve member health outcomes and lower costs.